What are the symptoms and causes of Diabetic Retinopathy?
Diabetes is a chronic disease that affects millions of people in the United States and around the world. People with diabetes, however, are at risk for a variety of additional health problems, including eye damage.
The most frequent type of diabetic eye illness is diabetic retinopathy. It’s a serious eye condition that, if not diagnosed and treated early enough, can lead to blindness.

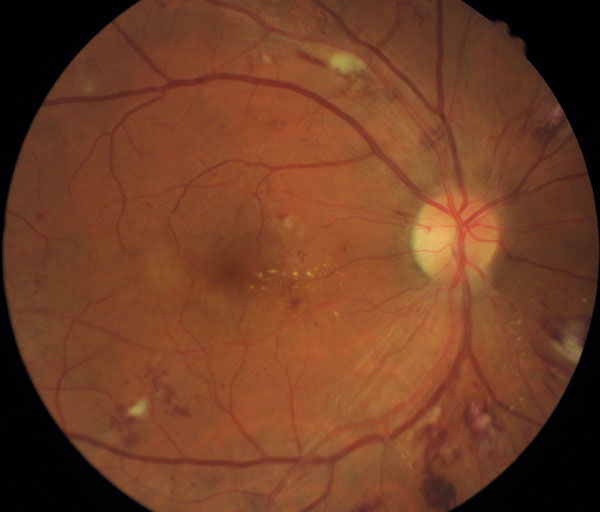
The retina (which is involved in diabetic retinopathy) is important for vision. It receives light that enters our eye and transmits information to our brain, allowing us to see. High blood sugar levels in patients with diabetes and even pre-diabetes can cause the tiny blood vessels in the retina to leak fluid or bleed. This can have an impact on and impair vision. Abnormal blood vessels in the retina can grow in quantity in people with diabetes, causing scarring and visual loss.
Knowing more about diabetic retinopathy can help you prevent the problem and safeguard your vision if you have diabetes or pre-diabetes.
The five most significant facts concerning diabetic retinopathy are shown below.
1. Diabetic Retinopathy is divided into four stages.
The phases of diabetic retinopathy are commonly divided into four categories. Mild nonproliferative retinopathy is considered the first stage. Swelling develops in the retina’s small blood vessels during this stage. Symptoms are almost never present. It’s possible that no changes are noticeable at this stage of the disease. To detect the early signs of diabetic retinopathy, regular eye exams are required.
The second stage of nonproliferative retinopathy is known as moderate nonproliferative retinopathy. Some of the retina’s blood arteries may become blocked, reducing the amount of nutrients and oxygen delivered to the retina. It’s possible that no symptoms will appear, and your vision will be unaffected. Regular eye exams are required to detect the indications of diabetic retinopathy as it progresses.
Severe nonproliferative retinopathy will develop if the situation worsens. New aberrant blood vessels form as additional blood vessels become occluded. Fluid can seep from them, causing the macula to expand and thicken. This swelling and thickening obstructs vision, making diabetic retinopathy symptoms more visible.
Proliferative retinopathy is the final and most severe stage of diabetic retinopathy. During the fourth stage, an increasing number of blood vessels become obstructed, and more aberrant blood vessels emerge, potentially resulting in hemorrhage in the eye’s center. Macular edema (swelling of the macula, which is important for fine vision), retinal detachment, and vitreous hemorrhage (swelling of the vitreous) are all possible consequences at this stage. More severe visual problems, such as blurred vision, flashes of light in the central vision, and black spots, can result from these changes.
2. Diabetic Retinopathy Doesn’t Always Have Symptoms
Because diabetic retinopathy is generally asymptomatic in its early stages, regular eye exams are essential. You should schedule a yearly eye exam with an ophthalmologist who specializes in diabetic eye disease if you have diabetes or pre-diabetes, even if you don’t have any symptoms of retinopathy. Special tests will be performed by an ophthalmologist who specializes in diabetic eye disease to detect diabetic retinopathy in its early stages, before symptoms appear.

Diabetic retinopathy symptoms often don’t occur until the condition has progressed to stage three or four. According to many clinics, as the condition advances, the following symptoms may appear:
- Vision is blurry.
- Vision loss that occurs suddenly
- Doubtful perception
- Floaters in your vision or spots in your area of vision
- In your field of view, there are dark regions.
- Night vision is poor.
- Changes in vision of any kind
3. Early detection could help to prevent vision loss
Diabetic retinopathy must be detected early in order to maintain vision. If symptoms are not addressed as soon as they are discovered, they can worsen. Severe vision loss or total blindness can occur over time. Vision loss can be avoided with early identification and treatment.

A full eye exam should be performed annually, or more frequently if any visual changes arise, to diagnose diabetic retinopathy early. To establish the health of your vision and eyes, your ophthalmologist will often perform the following tests during a full exam:
- A vision acuity test is used to assess your vision.
- A dilated eye exam helps your ophthalmologist to see the inside of your eye, particularly the retina, more clearly.
- Tonometry is a test that determines how much pressure is present inside your eye.
- A fluorescein angiography is a test that allows your ophthalmologist to see the blood vessels in your eye in order to diagnose retinal problems.
- Optical coherence tomography (OCT) is a technique for evaluating the macula.
4. Diabetic Retinopathy Treatment Is Available
While diabetes and the facts concerning diabetic retinopathy may appear frightening and overwhelming, there is good news. Treatment for diabetic retinopathy is available and can help avoid visual loss, especially if identified early.
Treatment will most likely entail lifestyle adjustments as well as medications to lower blood sugar, blood pressure, and cholesterol levels, which may help slow the disease’s progression. Additional treatment, like injectable therapy, may be recommended in more advanced cases of diabetic retinopathy. Anti-VEGF medications are injected into the eye and serve to prevent or reduce the progression of the illness by blocking the hormone that encourages blood vessel growth.
In severe stages of diabetic retinopathy, laser therapy may be a possibility. A particular laser is used to eliminate damaged structures in the retina, sealing leaky blood vessels and inhibiting the development of chemicals that cause aberrant blood vessels to form.
Laser treatment may not be possible in some circumstances, such as vitreous hemorrhage, and surgery may be necessary. In such circumstances, a vitrectomy surgery may be performed. To restore vision, the surgeon removes the blood-filled vitreous gel from the middle of the eye.
5. It’s Critical to Control Key ‘Numbers’ and Make Important Lifestyle Choices to Avoid Diabetic Retinopathy
Controlling your blood sugar, blood pressure, and cholesterol levels are the greatest approaches to reduce your risk of getting diabetic retinopathy. Blood sugar levels that are too high can harm the retina. Eyes can be harmed by high blood pressure and cholesterol. Remember that diabetic retinopathy can affect persons with both type 1 and type 2 diabetes.
Managing your diabetes effectively necessitates the consideration of a number of things. Consult your doctor about how frequently you should check your blood sugar. Inquire with your doctor about an A1C test, which measures your average blood sugar level over the previous three months.

It’s also crucial to be aware of your various health indicators or figures. Make a strategy with your healthcare team to keep your weight, blood pressure, and cholesterol levels in check. It’s also crucial to stick to your diabetes food plan, exercise on a regular basis, and take your medicine exactly as directed.
If you smoke, make an effort to stop. If you smoke, you’re more likely to get diabetic retinopathy. There are medications, nicotine patches, and smoking cessation seminars available to help you quit smoking.
Fortunately, if diabetic retinopathy is discovered early, it can be slowed.